 News
News
Auditor finds over $600,000 in improper payments to Medicaid…
Mississippi Division of Medicaid has made more than $600,000 in improper payments to the state’s contracted managed care companies, the state auditor’s office says.
Medicaid pays the managed care companies — UnitedHealthcare and Magnolia Health — a per-member rate every month to provide health insurance to nearly 442,000 Mississippians, over 70 percent of the state’s Medicaid population.
Many of the faulty payments occurred when the state continued paying the managed care companies for a member who had died or who was transferred to a long-term care facility, according to the auditor’s office Wednesday media release.
The agency identified 206 members who had died but remained on the rolls for extended periods of time. The total savings amount to some one-thousandths of one percent of what the state paid the managed care companies.
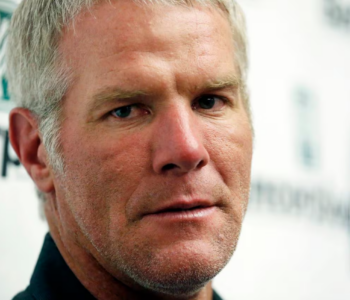
“We used new ‘big data’ techniques to identify these funds that were spent in error,” said newly appointed State Auditor Shad White. “Creating efficient government is a priority, and I am excited about the relationship my office has formed to ensure taxpayer dollars are being spent appropriately.”
The new technology increases the speed at which the auditor’s office is able to analyze extremely large data sets.
White touted the new partnership between Medicaid and the auditor’s office, which began under previous State Auditor Stacey Pickering, and commended Medicaid for its willingness to identify cost savings. Medicaid spokesperson Matt Westerfield said his agency initiated the auditing process as part of its “routine oversight” over the managed care companies.
“We continuously audit for errors in claims processing. In this case, the OSA offered to supplement DOM resources to assist in effectively identifying issues,” he said.
The auditor’s office and Medicaid are working to recoup the $616,447 in improper payments — out of several billion total — made during the time period June of 2014 to October of 2017, during which the managed care companies would have received several billion. Nearly $920 million of the state’s $6 billion budget is spent on Medicaid, which provides health care to nearly a fourth of the people in the state, mostly children.
Considering the size of the managed care program, $616,447 is a relatively small number of improper payments, White told the Clarion Ledger.
“In a way, it’s encouraging,” White said, because now the state has a tangible number and an idea of how to right set.
Medicaid said in the release that it is working on strengthening its protocol so improper payments are not processed in the future.
“We often collaborate closely with the Division of Medicaid on payment reconciliation, and adjustments are an ongoing process given the changing nature of Medicaid enrollment and eligibility,” said a statement from a UnitedHealthcare spokesperson. “We look forward to working with this new auditor and his findings.”
The state’s managed care companies, which will include Molina Healthcare of Mississippi come October, receive $3 billion in federal and state funds to run the MississippiCAN managed care program.
Because Medicaid pays the insurers a set amount upfront every month, as opposed to a fee-for-service model, the program provides budget stability for the state. The program’s proponents also argue it’s designed to provide preventative care and keep members healthier on the front end, decreasing costs on the back end.
Some officials have questioned whether the program has met either of those goals: better health outcomes or savings.
Medicaid says managed care has saved the state roughly $300 million in prevented costs since it began in 2011. In March, the agency announced it had saved nearly $5 million in one year by identifying unnecessary, expensive prescriptions covered by the state’s Medicaid program.
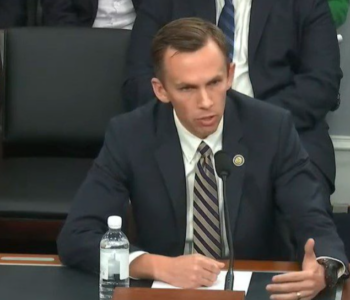
“I believe being responsible stewards of taxpayer dollars is one of the highest duties of any state agency,” Medicaid Executive Director Drew Snyder said in the release. “I appreciate the good work that the State Auditor’s Office and the team at Medicaid have done and continue to do in identifying and preventing payment errors.”